A guest blog post Karen Ashforth, OT MS CLT-LANA.
[This is a 25-minute read.]
Thank you for joining us for the fourth article in the “Understanding Fibrosis” series. In the first article, we looked at the basics of fibrosis, and its link to lymphedema. Then, we examined the types of fibrosis and treatment in phlebolymphedema and breast cancer-related lymphedema.
This article will cover the types of fibrosis and treatments for lipedema. This information is intended for educational purposes, and these treatments should be prescribed and administered by qualified professionals.
What is Lipedema?
Lipedema, sometimes called “painful fat syndrome,” is a chronic condition primarily affecting women. Lipedema is characterized by a symmetrical, bilateral build-up of fat beneath the skin, known as subcutaneous adipose tissue (SAT).
SAT is normally present in people, but in those with lipedema it is inflamed, painful, and can grow progressively harder and larger. It is common to have hard and painful nodules within the lipedema SAT ranging in size from rice-like, to walnut sized, or even larger. Lipedema is most commonly seen in the lower half of the body, except for the feet, which stay normal sized in the early stages.
Onset of lipedema seems to be linked to periods of hormonal change such as puberty, pregnancy and menopause. In these transitions, women can feel particularly vulnerable about body image, and dealing with lipedema can affect emotional well-being.
Some of my lipedema patients tell me that they have trouble going outside their home because they feel so self-conscious. As a therapist, I feel it is important to not only provide education and treatment to empower my patients to manage their symptoms, but to also give emotional support and encouragement. I often recommend the many online resources for lipedema, which provide a wide array of education and support.
Although lipedema is related to lymphedema and many treatments are similar, it is critical for patients and professionals to understand the unique aspects of lipedema. The name “lipedema” literally means swelling in fat. It is important to address this swelling in each stage of lipedema. Swelling appears and responds differently in early vs. later stages.
In stage 1 lipedema, swelling reverses with leg elevation. When treated clinically, there may be limited measurable reduction in leg size. This is because the larger leg size may be due more to SAT than swelling, and SAT does not reduce with traditional lymphedema therapy. Despite this, it is still important to treat stage 1 lipedema because it can help with pain, lymphatic and vascular function, and prevent progression of this condition. Lymphedema can develop as this condition progresses and is called lipo- lymphedema.
What is Dercum’s Disease (Adiposis Dolorosa)?
Dercum’s disease is a related rare fat disorder that is characterized by painful lipomas in the SAT. Dercum’s disease is also more common in women than men, and usually occurs in adulthood. There may also be problems with obesity, memory loss, expressive communication, patches of bleeding under the skin, benign growths of blood vessels, digestive issues, joint pain, rapid heart rate, shortness of breath, sleep issues, migraines, heavy menstrual bleeding, depression, anxiety, and fatigue after activity.
How is Lipedema Different from Obesity?
Lipedema is different from obesity, although it is possible to have both. Lipedema is characterized by painful, inflamed SAT. In obesity there are deep fat layers as well as SAT, but the SAT is not inflamed or painful. Obesity is characterized by widespread fat over the entire body, with two major patterns of fat distribution: gynoid (pear shape) and android (apple shape). Because the most common presentation of lipedema is in the lower body, lipedema can be confused with, and mis-labeled, as gynoid obesity.
When the two are present together, obesity can worsen lipedema and should be addressed. Although calorie restriction can yield weight loss with obesity, it is not helpful for lipedema. This can be discouraging, because women with lipedema can use calorie restriction to lose weight and fat mass from the upper part of the body, but there is minimal reduction in the lower body. Having said that, there are dietary programs that have recently emerged that are helping lipedema.
Lipedema and Lymphedema: Similarities and Differences
Lymphedema occurs when there is some type of failure to the lymphatic system. In primary lymphedema the lymphatic system is congenitally malformed. In secondary lymphedema, the previously normal lymphatic system has become injured due to disease, surgery or trauma.
In contrast, in early stage lipedema, the lymphatic system is initially intact but slow. The veins are dilated and leak fluid, causing swelling that resolves with elevation. Symptoms of pain, SAT, and nodule formation can start before significant edema is noticed.
As lipedema progresses, chronic inflammation causes fibrotic damage: SAT and nodules grow larger and becomes harder. If the lymphatic vessels are damaged by inflammation and fibrosis, edema accumulates and patients may be diagnosed with lipo-lymphedema, or lymphedema secondary to lipedema. This risk for developing secondary lymphedema becomes greater in the later stages of lipedema.
Although lipedema is often confused with lymphedema and obesity, lipedema has unique characteristics that set it apart. It can be further confusing when lipedema is present with obesity and/or lymphedema. I’ve summarized some of the major characteristics in these lists, to show differences between lipedema, lymphedema and obesity:
Lymphedema:
- Gender: males and females
- Onset: any age
- Hereditary: primary lymphedema is hereditary, secondary lymphedema is not
- Areas affected: any part of the body including the head, torso, abdomen, often asymmetrical
- Body Mass Index (BMI): can be normal
- Pitting: present at any stage but mostly early stages
- Hand and feet: swelling present at any stage
- Kaposi-Stemmer’s sign: positive
- Painful: yes, in some patients
- Bruising: requires significant trauma
Obesity:
- Gender: males and females
- Onset: any age
- Hereditary: in some cases
- Areas affected: usually entire body, may have gynoid (pear) or android (apple) fat distribution
- Hands and Feet: affected
- BMI: elevated >30
- Fat distribution: both superficial (under skin) and deep (around organs)
- Diet: responds to calorie restriction, fat and weight loss generally occur throughout body
- Kaposi-Stemmer’s sign: negative
- Painful: no
- Bruising: requires significant trauma
- Can aggravate lipedema and lymphedema symptoms
Lipedema:
- Gender: almost exclusively females
- Onset: mainly at times of hormonal fluctuation: puberty, around childbirth or menopause
- Hereditary: often affects other female family members
- Areas affected: always bilateral (both sides), primarily lower body, upper body 30% time
- BMI: can be normal
- Fat distribution: increased fat under skin: subcutaneous adipose tissue (SAT)
- Hands and feet: not affected in early stages
- Kaposi-Stemmer’s sign: negative in early stages
- Diet: not responsive to traditional diet and exercise: with calorie restriction, weight loss usually occurs mainly in upper body
- Painful: yes, in almost all patients
- Bruising: easily bruised due to increased capillary fragility
- Hypothermia of skin
 What are the Different Types of Lipedema?
What are the Different Types of Lipedema?
Lipedema has five distinct patterns of increased SAT distribution in the body:
- Type I: Pelvis, buttocks and hips
- Type II: From buttocks, to knees, folds of fat on the inner knees
- Type III: From buttocks to ankles, “cuff” of tissue overhanging ankles
- Type IV: Arms and sometimes legs
- Type V: Legs/Knees to ankles, “cuff” of tissue overhanging ankles
What are the Stages of Lipedema?
Lipedema is a progressive condition that can become more serious if it is not treated. Because lipedema responds well to treatment in stage 1, the earlier it is addressed, the better.
Stage 1:
- Skin surface is normal
- SAT soft
- Nodules may be present ranging in size from rice-like to walnut-shaped
- Swelling minimal: (edema during daytime, resolves with elevation), hands/feet not affected
- Responds well to treatment
Stage 2:
- Skin surface becomes uneven and harder with “mattress pattern” indentations
- SAT hardens, indentations visible, larger
- Nodules increase in size, become harder, can become stuck together
- Increased daytime swelling, elevation less effective, hands/feet not affected
- May respond well to treatment
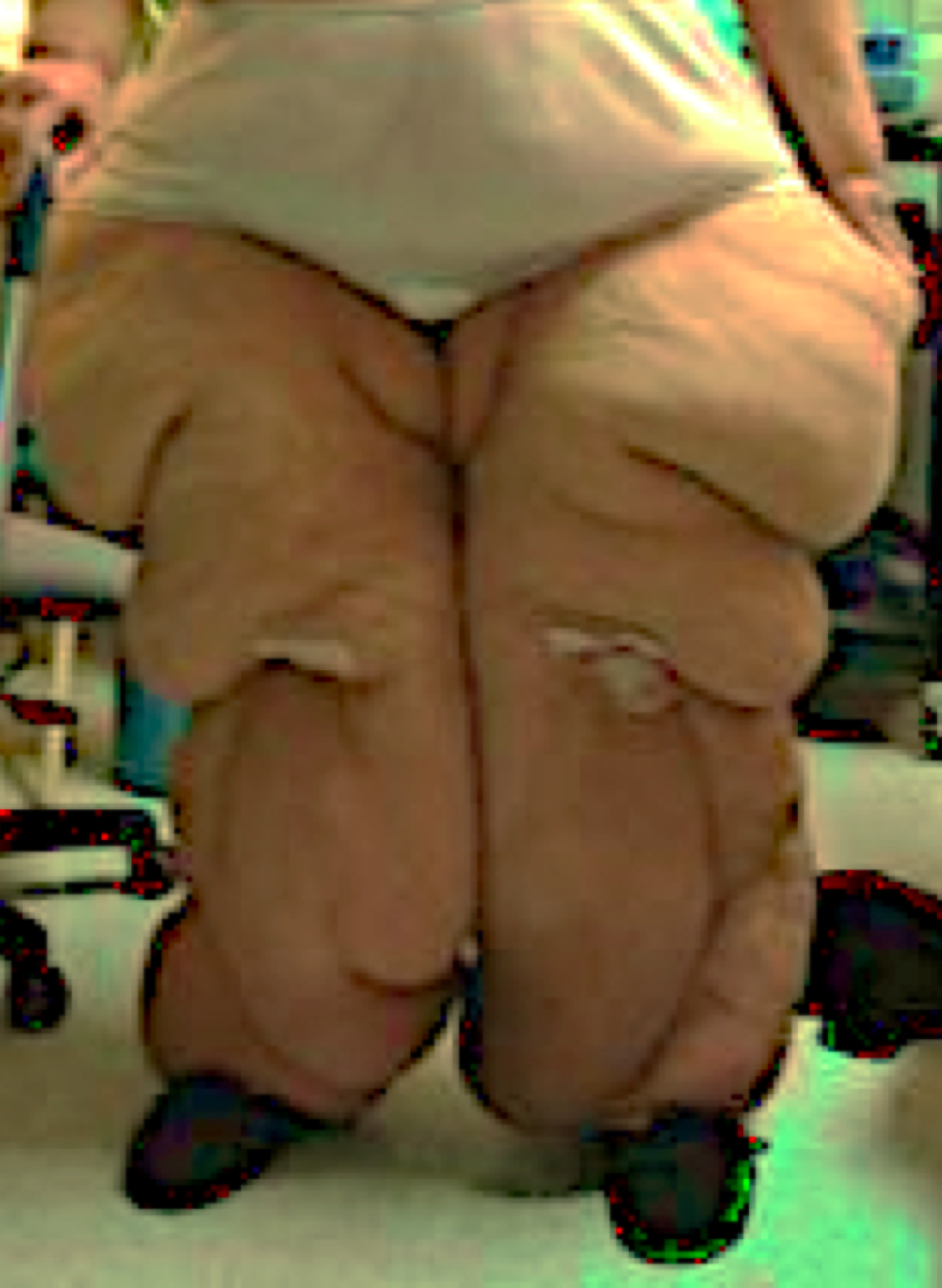
Stage 3:
- Skin surface thick and hard, peau d’orange, (orange peel-like quality),
- SAT increases and continues to harden
- Nodules are large
- Fat pads and lobules (large masses of tissue that overhang) especially on thighs, knees, and ankles
- Swelling present continuously, hands/feet generally not affected
- Less responsive to treatment
Stage 4:
- Also called Lipo-Lymphedema (lipedema with lymphedema)
- Very hard skin and SAT
- Multiple large masses of overhanging tissue
- Swelling present continuously including dorsal foot swelling, positive Kaposi-Stemmer’s sign
- Less responsive to treatment
Lipedema Treatment:
Complete decongestive therapy (CDT): is used to treat both lymphedema and lipedema. CDT consists of manual lymphatic drainage (MLD), exercise, compression bandaging, compression garments, and skin care. CDT helps lipedema by decongesting swelling, encouraging normal lymphatic vessel pumping, and decreasing pain.
Manual lymphatic drainage (MLD): MLD is a gentle massage that directs lymph fluid out of swollen areas and assists the body’s lymphatic drainage patterns. It is performed by a certified lymphedema therapist, who can also teach people with lipedema to perform it on themselves. MLD can be very relaxing, can decrease pain, and stimulate lymphatic circulation. MLD is known to decrease capillary fragility in lipedema. Applying compression garments after MLD help keep the reduction effects.
Compression bandaging and garments:
Compression bandaging can be helpful to reduce larger amounts of swelling. However, it may not be needed or tolerated in earlier stages of lipedema, where there are small amounts of swelling. In these cases, the majority of the bulk can be due to SAT, rather than edema.
Compression garments help to compensate for loss of skin elasticity and provide support to tissues. This can decrease pain and enhance muscle pumping action to move fluid out of swollen areas. They provide containment to maintain the reduction of swelling after MLD, and prevent fluid from reaccumulating. This helps the body feel less heavy and can make it easier to move and walk. Ultimately, wearing compression garments helps prevent lipedema from progressing to later stages by helping the lymphatic and vascular circulation.
It is important to strike a therapeutic balance between the amount of SAT, severity of swelling, and degree of compression, in order to maximize comfort in garments. Medical grade (>20-30 mmHg) compression garments may be painful to wear and difficult to put on and take off.
Textured circular knit compression garments have less compression (12-21 mmHg) but the micro-massage created by the weave in the fabric stimulates the superficial lymphatics, and compensates for having less pressure. They are also generally more comfortable to wear and easier to put on and take off, but may not be strong enough to support larger bodies or stage 3 and 4 lipedema. In those cases, custom elastic flat knit or Velcro wraps might be better compression alternatives.
Types of compression can be layered, or different garments can cover different parts of the body depending upon need. For instance, it is possible to achieve a compression gradient and comfort using a textured elastic capri garment to compress the hips, thighs, and knees with lower legs compressed by Velcro wraps or medical grade custom flat knit elastic compression stockings. Quilted compression can also be effective, but it is bulkier and hotter to wear.
A caution: if compression is only used on swollen areas that are closer to the trunk such as thighs and knees, the uncompressed lower legs and feet are vulnerable to increased swelling.
Exercise: This is very important because the lymphatic system relies on the pumping action of muscles to move fluid. Deep breathing and muscle contraction increase oxygen in the body’s tissues, and hypoxia (low oxygen) is thought to be an important factor in lipedema. Deep water exercise is particularly beneficial for those with lipedema. Hydrostatic pressure and buoyancy can enhance the muscle pumping action, help prevent injury, and decrease weight on the joints during exercise. However, over exercising is harmful to SAT tissues by building up lactic acid and oxidants.
Skin Care: It is important to keep the skin moisturized and healthy: this creates a good barrier to prevent infection.
Elevation: Elevating legs periodically during the daytime helps harness the effects of gravity to help with orthostatic swelling that occurs in stage 1 lipedema. It can also be helpful in later stages when combined with more aggressive treatment.
Pneumatic compression: If conservative treatment of elevation, compression, and exercise do not yield significant changes in swelling, pneumatic compression can be helpful. During pneumatic compression, patients put on an appliance that contains individual air chambers and the chambers inflate sequentially from the hands or the feet towards the trunk.
There is much research to support the benefits of pneumatic compression for lipedema and lymphedema. Evidence points not only to pneumatic compression stimulating lymphatic circulation and reducing swelling, but also to pain reduction as well as decreasing capillary fragility in lipedema.
An additional benefit is that pneumatic compression promotes relaxation.
Many insurances pay for this equipment for home treatment. There are a number of options for pneumatic systems, including those which accommodate larger sized people. The ability to adjust the pressure and programming to find both comfort and effective treatment is important.
Nutrition:
Lipedema SAT is not responsive to calorie reduction, and in the past, lipedema was believed to not be affected by diet at all. In the last few years, two groups of experts in lipedema have emerged with guidelines that are proving effective in helping lipedema.
Both groups acknowledge the unique characteristics of lipedema fat, and how it differs metabolically from “regular” fat. Regulating insulin production and normalizing estrogen levels appear to have marked effects on both regular and lipedema fat. These books represent two approaches that offer dietary choices to lower inflammatory, hormonal and metabolic factors in lipedema and lymphedema:
Lymphedema and Lipedema Nutrition Guide (2016 Ehrlich et al) is authored by physicians and clinicians specialized in lipedema and lymphedema treatment. It includes specific guidelines about recommended eating patterns that “starve” lymphedema and lipedema. Emphasis is on eating whole foods, limiting animal protein, and avoiding refined grains, added sugars, most dairy products, and chemically modified fats. Specific nutritional supplements are recommended.
The Ketogenic Solution for Lymphatic Disorders (2019 Keith) is written by an occupational therapist and certified lymphedema therapist who earned her doctorate studying the effects of the ketogenic diet with lymphedema and lipedema patients. The ketogenic diet has been in use for over a century and is supported by a wide body of research. Guidelines emphasize specific proportions of healthy fats, proteins, and limited low glycemic (low sugar/starch) carbohydrates.
Although there are no specific studies published regarding effects of these nutritional guidelines with lipedema patients, anecdotal reports from some women following the ketogenic diet state that they have lost fat and inches from their lower bodies for the first time in their lives. Some women report that SAT becomes softer, while others have experienced nodules becoming more prominent, suggesting they experienced loss of SAT but not nodules.
 Why Introduce Antifibrotic Treatment Gradually?
Why Introduce Antifibrotic Treatment Gradually?
As with lymphedema, fibrosis is present in all stages of lipedema, but the types of fibrosis are unique to lipedema. Therefore, special approaches and techniques are necessary to address lipedema fibrosis. Lipedema fibrosis can be further complicated by other types of fibrosis such as surgical scar tissue, radiation-induced fibrosis, post-cellulitis fibrosis, or lipodermatosclerosis. Specific treatment for those types of fibrosis have been discussed in previous articles in this series.
One of the biggest caveats is to work within pain tolerance and not try to be too aggressive right away. The deeper and more aggressive treatments used for lymphedema-related fibrosis can be more painful, and create more bruising when used with lipedema-related fibrosis. If approached gently, many lipedema patients are willing to trade the temporary pain and bruising side effects in exchange for softer, lighter tissues, as well as increased function and mobility.
Fibrosis treatment will be more successful if any swelling is addressed first. After performing decongestion, anti-fibrotic techniques can be introduced gradually, in small doses. Educating the lipedema patient about types of treatments, and the benefits of each can build trust, and encourage participation.
These techniques are highly specialized and not taught in basic lymphedema training programs. It is important that practitioners be experienced in lymphedema and lipedema treatment, and also be properly trained in advanced techniques before incorporating them into treatment.
How is SAT different from lymphostatic fibrosis?
In the first article of this series, we discussed lymphostatic fibrosis: how it is a fatty matrix created by an inflammatory process in chronic swelling. Lymphostatic fibrosis begins as a high protein accumulation of swelling that gradually attracts fat cells, which promotes conversion of liquid edema into fatty tissue. The underlying causes and development of lipedema SAT are still speculative. The damages to SAT in lipedema are thought to be influenced by estrogen regulation, which affects the body in a number of ways.
These include widespread inflammation which impacts sensory nerve pain, metabolic changes, leaky blood and lymphatic vessels, tissue hypoxia, presence of VEGF (which stimulates new, but abnormal blood vessel growth), and abnormal quantity and size of fat cells. The easy bruising in lipedema is a result of the fragility of capillaries in the SAT. The inflamed SAT in turn produces scar tissue in an attempt to repair itself, creating fibrosis.
This fibrosis adheres to the skin, as well as bones, muscles, tendons and ligaments. The end result is a vicious cycle of inflammation, producing dense, hard tissue, that creates more abnormal fat tissue. The fibrotic obstruction and impaired circulation increase swelling and nerve compression, which, in turn, can create pain.
What are SAT Tissue Nodules?
Fibrosis forms around the subcutaneous fat cells, creating nodules. These can range in size from a grain of rice to the size of walnuts, or even larger. If lipedema progresses, the nodules can adhere to each other and the SAT, creating large, lumpy, painful masses. In later stages of lipedema, large pendulous lobules can form, which can make it challenging to find well-fitting clothing, and may interfere with sitting, standing or walking.
Specific Anti-Fibrotic Treatments:
Having a large toolbox of techniques allows practitioners versatility in treatment. Some techniques are gentle and others are very aggressive. After swelling is addressed with CDT, these techniques literally go deeper, and can provide significant results. As with lymphedema-related fibrosis, “tune-ups” may be needed. Depending upon the individual and the technique, it may be appropriate to incorporate some fibrosis treatments into the home program.
Manual therapy: There are anti-fibrotic manual therapy techniques for lymphostatic fibrosis that can be helpful for lipedema fibrosis. Some CDT training programs teach deeper manual techniques. Other deep tissue massage techniques, such as myofascial release, or the Chinese massage technique of Tui Na, can be helpful in treating fibrotic SAT and nodules.
Of interest is a technique specifically directed towards SAT, called “Quadrivas therapy.” It is practiced exclusively in the Netherlands. Quadrivas is a full body treatment that softens SAT nodes and masses. Treatment begins superficially by softening SAT, then pressure deepens over subsequent treatments to address muscle and fascia layers all the way to the bone.
Dr. Karen Herbst studied this technique over a four-week period in 2017, with a group of seven women with lipedema. Effects of the treatment were significant, and included decreased fibrosis, pain, leg volume and body fat. Some participants also experienced improved SAT structure. Treatment side effects found during the study were pain, bruising and heartburn.
Despite that, all participants said they would recommend this treatment to women with lipedema. Although the pilot study was small, it demonstrated that aggressive techniques were effective in helping lipedema-related fibrosis. A seminar for certified lymphedema therapists was offered in the same time period as the study, and opened the door for lymphedema practitioners to successfully incorporate more aggressive anti-fibrotic techniques into lipedema treatment.
Compression:
There are many types of compression garments and pads that have anti-fibrotic effects. Textured elastic compression garments (either non-medical grade or custom flat knit) can provide a gentle anti-fibrotic effect to hardened skin, SAT, and nodules. Bulkier quilted compression with more irregularly textured filling, such as chipped foam, foam strips, or cherry pits, can be useful. These pads and garments can be gentle or aggressive depending upon the medium and the amount of pressure used over them.
It should be noted that cherry PitPaks must be used cautiously with sensitive skin, or altered sensation. For patients with high levels of pain, PitPaks are best used for a brief trial of 30-60 minutes with a skin inspection and pain assessment before using for longer periods. PitPaks or chip foam quilted compression pads may be placed inside of other compression garments to address hardened areas of tissue. Quilted garments cover a much wider area than pads, but are bulky and may be best suited to wearing at night or during pneumatic compression treatment.
Low level laser: The anti-inflammatory and anti-fibrotic effects of near infra-red (non-thermal) light therapy are useful prior to and along with manual or instrument techniques. The aperture of the laser can even be used as an anti-fibrotic instrument while delivering light therapy.
TENS (transcutaneous electrical stimulation): This modality has been used medically for decades to lower pain and inflammation. On certain settings (extremely low frequency), it can stimulate the body to produce endorphins, which help to control pain. TENS was shown to help reduce pain, reduce SAT, and increase function in a single study of a man with Dercum’s disease. Because of the anti-inflammatory effects of TENS, it may be a potentially useful treatment for rare adipose disorders.
Vibration: This has been shown to stimulate vascular and lymphatic circulation, reduce pain, and reduce inflammation in people with lymphedema. It can also be useful for those with lipedema, and with proper training, can be a good addition to the home program. Hand held vibrators have historically been used clinically to remodel many different types of hardened scar tissue. Whole body vibration has been found to be an effective treatment for lymphedema and lipedema.
Elastic taping: This is used widely in many medical settings, including treatment for lymphedema, sports injuries and neurological conditions. Benefits include pain management, edema management, scar tissue remodeling, posture management, and neuromuscular facilitation. A specialized, highly adherent tape “lifts” skin to improve superficial circulation.
The mechanical pull of the tape creates gliding of adhered tissues to soften fibrosis. It is very important to determine skin tolerance prior to treatment to avoid irritation. Tape must be removed properly to avoid tearing skin. Taping can cover large areas of SAT fibrosis, and is useful for providing support, and decongesting fat pads and lobules. There are many applications, techniques, caveats and contraindications which make special training essential.
Instrument assisted soft tissue mobilization: This technique is based on the Chinese “Gua Sha” treatment which traditionally uses ceramic or jade instruments to provide a deep massage to tissues. It is also known as Graston Technique, Sound Assisted Soft Tissue Mobilization or Astym. There are now many different variations of the basic technique, with tools ranging from surgical steel to plastic.
This treatment creates a controlled microtrauma that remodels tissues. Techniques can range from very gentle to very aggressive. Side effects can include pain, bruising, and petechiae (broken blood vessels). When instrument massage is performed for people without lipedema, these side effects usually resolve within 48 hours, but they can last much longer if performed on lipedema fibrosis due to fragile vasculature. Because of this, it is critical to have proper training in these techniques, as well as to use caution, and monitor side effects.
Negative pressure: This is based on traditional Chinese medicine “cupping.” This technique relies on a gentle suction that lifts and separates layers of tissue that are stuck together. Like instrument massage, this technique can create a controlled microtrauma to remodel tissues, and has similar potential side effects of pain, bruising, and petechiae. Some specialized negative pressure equipment can offer a variety of calibrated and controlled pressures as well as adjunctive treatments such as vibration. Negative pressure should never be attempted without training, and should not be used aggressively with lipedema.
Hivamat: This is an oscillating electrical modality used in lymphedema treatment, and has been studied as a decongestive agent for lipedema. It is gaining popularity clinically for treatment of many different types of lymphedema and lipedema-related fibrosis.
Pneumatic compression: While most people think of pneumatic compression as a decongestive treatment, it can also be a powerful anti-fibrotic agent. Using chip foam pads or garments during a pneumatic compression treatment can create a gentle effect that can soften tissues progressively as treatment is repeated over time. Some patients are able to tolerate PitPaks under pneumatic compression, but this treatment is very aggressive. It is advised to determine tolerance first, before using PitPaks with pneumatic compression.
Using higher pressures can create a deeper and more powerful treatment. Higher pressures may be required to give a therapeutic treatment in the later stages of lipedema if tissues are hard and bulky, or if obesity is also present. Pressure should always be adjusted to tolerance.
Most pneumatic compression devices have the capability for one or both types of commonly used compression programming: sequential and peristaltic. Both programs start the cycle of inflation at the hands or feet and chambers are inflated, moving in the direction of the torso. With sequential programs, each chamber stays inflated until all chambers are inflated, and then all deflate at the same time before starting a new cycle. In peristaltic programs, only 1-2 chambers are inflated at a time, forming a wave-like action.
Peristaltic programming is generally more comfortable for people with lipedema, especially if higher pressure is required to move fluid through bulky tissues and remodel fibrosis. As fibrosis softens and tissue volume decreases, less pressure may be needed. It is important to make sure that pressure is always regulated to a comfortable level.
Sequential programs can be used if peristaltic is not available, but overall pressure may need to be lowered if hands or feet are uncomfortable from the sustained pressure held through the entire cycle. A way to minimize this problem is to select a pneumatic compression device that has a rapid cycle time and longer pause time, to avoid prolonged pressure on hands and feet.
There are a number of different appliances used with pneumatic compression.
Type I, II, III lipedema: A pantsuit appliance that treats both legs, groin, hips, buttocks, and abdomen is most appropriate. Some appliances that treat legs and abdomen have a gap in the crotch, leaving the genitals and lower buttocks without treatment, and increasing the risk for developing more swelling and fibrosis in these areas. Larger appliances are available for those with later stages of lipedema, or a combination of lipedema and obesity. These must be used with specialized pumps that are capable of inflating larger appliances.
Type IV or V lipedema: If swelling is only present in the lower legs, leg sleeve appliances are appropriate, but if swelling progresses to the thighs, a pantsuit appliance is the best choice. For arms, a jacket-style appliance is best, particularly if swelling is present in the upper arm and axilla region.
The success of the treatment is affected by how well the appliance fastens and conforms to the body. Some pumps have sensors that work with zipper-closure appliances that give feedback during inflation to deliver the specified dosage of compression while inflating to fit, conforming evenly around the body.
Velcro-closure appliances rely on the ability of the user to close the Velcro correctly each time to conform to body contours. The entire appliance must be closed correctly to prevent areas of irregular pressure, which could leave untreated areas vulnerable to filling with pockets of fluid. Additionally, if fastened loosely, the treatment will not deliver the specified pressure.
With either type of closure, patients with large lobules or large variation in diameter within a limb may need to use padding, as is done with compression bandaging. Towels or small pillows make effective padding to ensure even compression with irregularly shaped limbs.
Therapy balls: Soft and hard balls come in small and large sizes, and can even have surface texture. They can be used to treat fibrosis by using the weight of the body to “melt” tissues against the ball. Pressure is controlled by body posture. The most control and least amount of pressure is achieved while standing with the ball between the body and a wall. There is extreme pressure when lying on the ball either face up or face down. Pressure can be static or dynamic: the body can rest against the ball or move back and forth to create a massaging effect. Hard balls should not be used for more than 60 seconds due to potential bruising.
Foam rollers: Foam rolls are available in different sizes and textures. They can cover a large surface area, and also be used in numerous positions to create a self-massage to fibrotic areas. Foam rolls made from hard closed-cell foam may create more discomfort than soft balls, and should be approached cautiously.
Surgery:
Liposuction has become increasingly popular as a means of removing lipedema SAT and is now covered by some insurances in the US. Lymph sparing liposuction techniques, such as tumescent liposuction or water jet assisted liposuction, are preferred for lipedema and lymphedema over traditional liposuction and debulking surgeries. These specialized techniques are more efficient at removing SAT, have fewer side effects, and are less likely to damage lymphatic vessels.
Longitudinal studies of up to eight years post-surgery have demonstrated sustained improvements in size, swelling, pain, heaviness, function and quality of life. However, liposuction cannot completely remove all lipedema SAT and it is possible that remaining tissue can grow over time and, in some cases, even return to prior symptoms. It is also possible to develop lymphedema as a side effect of liposuction. It should be noted that those with Dercum’s disease who have SAT excision have a 50% likelihood of recurrence of SAT.
The Impact of Fibrosis Treatment on Lipedema:
Going beyond basic lipedema and lymphedema treatment can be invaluable for individuals with lipedema. Anti-fibrotic treatment to remodel SAT and lobular fibrosis can impact lymphatic and vascular circulation, pain, mobility, body size, and may help prevent the progression of lipedema. Providing empowerment with education, clinic treatment, and an effective home program can create hope and a higher quality of life.
About the Author
Karen Ashforth, MS, OTR/L, CLT-LANA has practiced as an occupational therapist for 38 years. Specializing as a board-certified hand therapist led to her interest in lymphedema and fibrosis nearly 20 years ago. Karen’s passions in lymphedema practice are equipment innovation and development, treatment of underlying fibrosis and inflammation, and assessment of complex and difficult cases.
She is considered an expert in clinical use of pneumatic compression and has participated in the development of numerous devices and appliances. She currently works at St. Joseph’s Medical Center in Stockton, California, providing outpatient lymphedema treatment and also has a private consulting practice.
Karen speaks frequently at academic, clinical and professional settings and performs clinical research that she presents and publishes nationally and internationally. She is also an adjunct faculty member with the University of the Pacific in the Doctoral Physical Therapy Program.
